What’s Up Doc? Tips to Avoid Medical GasLighting by Shannon Cramer
“Hypochondriac: Overly-anxious. Attention seeker.” I was called all of these names during my twenties when I was searching for answers to my debilitating fatigue.
Despite sleeping fourteen hours a day, I woke up just as tired as when my head hit the pillow. This wasn’t me. I was the active honor roll student who couldn’t wait to build a life with the amazing man I had just married.
As if a switch had flipped, I was struggling to have enough energy to work part-time, see friends, go to the grocery store, or even shower. Forget exercise, hobbies or thinking about kids! I was a real-life zombie–and yet medical professionals routinely downplayed my symptoms as being “in my head.”
I wish I could say this type of medical gaslighting is an unusual experience for people with invisible illnesses. But there are thousands of stories like mine. Doctors see young people who look healthy on the outside, are stumped by their symptoms, and preventable damage is done when these patients are written off as time wasters.
Eventually, I was diagnosed with two very “real” physical disorders: narcolepsy and POTS. Narcoleptics function at the energy levels most people would experience after 24-48 hours of sleep deprivation because our bodies have lost the ability to regulate the quality of our sleep. This diagnosis happened fairly quickly.
POTS (post orthostatic tachycardia syndrome) is a communication disorder between the brain and autonomic nervous system. It causes extreme fatigue due to rapid heart rate, blood pressure dysfunction, and (in my case) a constant battle of dehydration because of low blood volume. It also wreaked havoc on my digestive system! I spent over five years seeking help from a gamut of specialists before a wonderful doctor pinged that I also had POTS.
For all of my brothers and sisters still searching for answers, here are some common sense observations and hard-won lessons that finally helped my doctors sit up and pay attention:
1. Be on time and prepared.
EVERY MINUTE MATTERS for medical zebras with complicated medical conditions. Most physicians see 11-20 patients a day. The average time spent with each patient is 17-24 minutes. While experts suggest that the ideal patient load for a primary care doctor is around 1,000 patients, doctors report that their patient load is closer to 2500.
Respect the time of these extremely busy professionals and the patients coming after you. If you are late, you don’t just hurt yourself–you take away from other patients. Think through how you are going to make the most of your extremely limited time with your physician:
- Leave early to allow plenty of time for traffic.
- Fill out your paperwork and check in on the portal ahead of time.
- Write down the key points you want to share about your symptoms at home when you can think about distractions.
- Bring your meds or a detailed list of your medications so that you’re not wasting time trying to remember names or dosages.
- Drop off copies of pertinent results you want to share (that have been performed by other doctors) before the day of your appointment. Your physician may be able to review them and come into your appointment with an idea of what’s going on.
- Have a list of questions ready. Discuss your talking points with a family member or close friend familiar with your situation to ensure you aren’t missing anything.
2. Dress to impress.
It is human nature to pay attention to looks. When you take time to put yourself together. You send an unconscious message to others that your time is valuable. Over 13-plus years of chronic illness, I’ve noticed that when I dress to impress, doctors are more likely to listen, less likely to dismiss my conclusions, spend more time with me, and are more invested in my case. Who would you naturally defer to? Is it a person in professional dress or someone who looks like they just rolled out of bed?
3. Bring backup.
I bring my husband to all of my most important appointments. My job is to present my case clearly to the doctor, and Parker’s job is to take notes on everything the doctor says. Practically, this helps us absorb everything that is happening and positions Parker to support the complexities of my care better. But having him there also serves another purpose.
It shocks me that many male (and female) doctors still value the word of a man over a woman. Having another person there to say, “She is not crazy; this is a huge issue that significantly impacts her quality of life; here is what I see..” is tremendously valuable. Parker provides another perspective that validates my experience.
Additionally, some doctors do not respond well to emotionalism. While it is perfectly natural to be upset about chronic illness, these doctors will respond better to an advocate who can more objectively discuss your condition—tag team with a spouse, parent, sibling, neighbor, or close friend.
4. Be specific about your symptoms. See examples!
Doctors are data-driven scientists: So don’t be vague about your symptoms. Put a number on it if you can. If you can’t, use specific examples to paint a picture. Even better, take a picture or a video! Here are a few examples from my appointments:
WEAK: “I’m losing weight.” STRONG: “I have lost another 14 pounds in the last three months without trying. I can’t eat more than a cup of food at a time.”
WEAK: “I’m uncomfortable all the time from bloating.” STRONG: “Here are two pictures. The first one is before my stomach issues. I weighed 150 pounds, but my stomach was relatively flat. Here is a picture of me after eating a cup of soup a few nights ago. I now weigh 140 (10 pounds less), but see how bloated I am in comparison? I look seven months pregnant.”
WEAK: “I’m always tired.” STRONG: “I’m so tired that I have trouble doing basic tasks like brushing my hair, walking to the bathroom, or getting off the couch to get something to eat.”
5. Treat the entire team with kindness
Outside of the doctor’s office, it is the doctor’s team that shoulders most of your care. Nurses read and respond to patient portal messages, organize the paperwork for refilling prescriptions, and help run things by insurance. Receptionists relay messages, keep an eagle eye on appointment availability, and watch over the waitlist.
When you are at your doctor’s office in person, be kind enough to be memorable. Ask the receptionist about their day. Say, “Thank you.” Genuinely compliment your nurse to their boss. Little kindnesses can go a long way in our fast-paced world when people are too busy to notice others. When you have a positive relationship with the entire team, people will be more willing to advocate for you when you need to be squeezed in for an appointment or to have a prescription filled pronto.
6. Believe in yourself–you know your body best.
Trust your gut. Doctors consider me one in a million. Even with my rare disorders, some of my symptoms present atypically. Medical professionals are trained to look for the most likely solution. When your symptoms are unusual, it is crucial to believe in yourself. I learned this lesson the hard way with my POTS digestive symptoms.
I developed a chronic cough at the age of 24. Not an occasional polite clearing of the throat–hundreds of episodes of violent coughing a day until I gagged. After ruling out asthma and dismissing the idea of reflux(I didn’t have heartburn), my doctor suggested I might have a “nervous” cough. That screwed with my head. The cough WAS worse in public situations when I was nervous about being disruptive.
I spent five months second-guessing myself because of what one doctor said. After all, she was the one with the medical degree. When I couldn’t stand the misery anymore, I got a second opinion. I was sent to a gastroenterologist who did an endoscopy and diagnosed me with Barrett’s Esophagus. I had GERD (acid reflux) but was in the minority of patients who didn’t have heartburn. The reflux had eroded a spot in my esophagus to the point that the cells were beginning to mutate. It is a precancerous condition that is easily treatable as long as it is monitored.
So, if you feel something is wrong, trust yourself. Be polite but firm. If a doctor is not taking your concerns seriously, get a second or seventh opinion. If a provider admits something is wrong but doesn’t know how to help (something I can respect), ask them to refer you to someone who can.
7. Trust yourself into the hands of the ultimate advocate
In my 13-plus years with chronic illness, there have been times when I have come to the end of my strength, weary to the bone, and have exhausted my medical options with no clue where to turn. But, in these moments of great weakness, God has never failed to come for me. I’ve seen Him move us next to a neighbor with the same rare medical condition who was able to connect me to a game-changing doctor, open up 18-month appointment waiting lists, work insurance miracles, and empower me to love my life despite chronic illness.
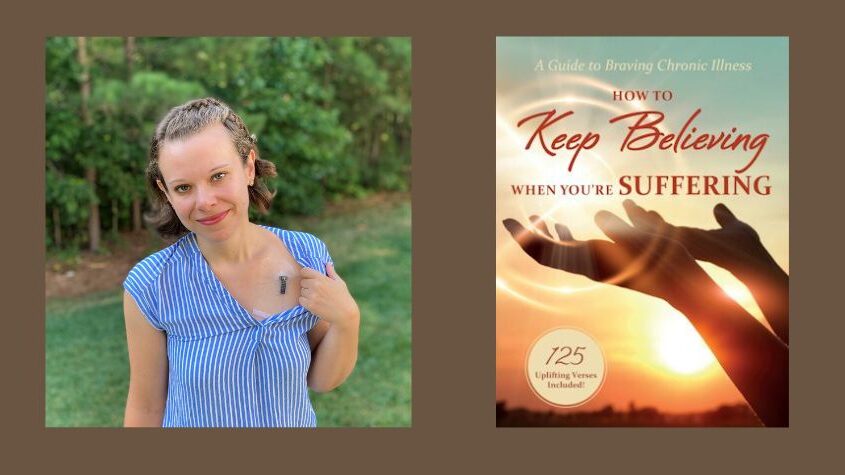
Need biblical tools to reconcile tough questions about suffering and fuel your faith? Want to learn more about Shannon’s experience of seeing Jesus work wonders in her life? Check out her book, How to Keep Believing When You’re Suffering: A Guide to Braving Chronic Illness, available on Amazon.
Jesus will come for you, too. He already became fully human, so he would know exactly what it is like to walk in your shoes (Hebrews 2:17). As the risen Christ, he has made it HIs job to intercede for you (Hebrews 7:25). So, take heart! The resurrection king is in your corner. His thoughts surpass all human wisdom, and His vision is not limited by what blinds us. NO law of nature or man can bind him. His specialty is the impossible–because Jesus is the Ultimate Advocate.




